Spinal stenosis is one of the most common spinal disorders. It often occurs in the lower back, and was first mentioned in the field of medicine around 200 years ago.
What are the causes?
Spinal stenosis occurs due to the degeneration of the spinal discs that occurs with age. The discs lose their cushioning ability and become thinner, causing the facet joints in the back of the spine to enlarge, while there is also a thickening of the tissues surrounding the nerves. These factors contribute to the narrowing of the spinal canal, although age, genetics, and lifestyle factors also play a role in the development of the condition.
Symptoms
Within the spinal canal, there are nerves that control various muscles and provide sensation to the skin along their distribution. When the spinal canal narrows significantly, it compresses the nerves within it, leading to symptoms such as back pain, radiating pain down the legs, numbness, or weakness. Some people may also experience difficulty controlling bowel movements.
Who is affected?
Spinal stenosis is most common in individuals over the age of 50 and it affects both men and women equally. It is more prevalent in individuals who engage in activities that put stress on the spine, such as heavy lifting or frequent bending and twisting, with other risk factors including a family history of the condition, obesity, and smoking. In younger individuals, the condition may be present from birth if there is a congenital narrowing of the spinal canal, making them more susceptible to nerve compression even from minor abnormalities in the spinal canal.
How is it diagnosed?
The diagnostic techniques employed depend on the patient's unique situation. During the physical examination, the presence of pain or weakness in the muscles innervated by the affected nerves may be detected. An x-ray may reveal degenerative changes in the spine, such as disc thinning and facet joint enlargement, while some individuals may also have signs of spinal instability. Magnetic resonance imaging (MRI) is a diagnostic tool used to confirm the condition, as it allows visualization of the spinal nerves and the areas where they may be compressed. It also helps assess the severity and location of the compression.
Treatment
In individuals with mild symptoms, it is recommended that they modify their lifestyles, including avoiding heavy lifting, reducing body weight, and strengthening the back muscles. Medication and physical therapy can also be combined into a treatment plan.
For individuals with severe symptoms, such as significant leg pain, difficulty walking even short distances, and significant disruption of daily life, surgery is an effective treatment option. Currently, there are various surgical techniques available, depending on the suitability for each individual patient.
- Microscopic or endoscopic surgery involves removing the tissues and bones that compress the nerves. This approach utilizes small incisions, resulting in minimal tissue damage and less postoperative pain. Hospitalization is brief, and recovery is relatively quick.
- Fusion surgery involves inserting metal implants while removing the tissues, bones, and nerves causing the compression. This method is suitable for individuals with severe back pain resulting from joint degeneration, deformity, or spinal instability.
In conclusion, spinal stenosis is a common condition that involves back pain or pain radiating from the hips down the legs. It is particularly common in older individuals or those exposed to risk factors, with accurate diagnosis reliant on symptom assessment, physical examination, and radiographic imaging. Treatment aims to improve quality of life through lifestyle modifications, medication, physical therapy, and surgery, depending on the patient's symptoms and needs.
Article by Dr. Pritsanai Pruttikul
Specialist in orthopedics and spinal surgery
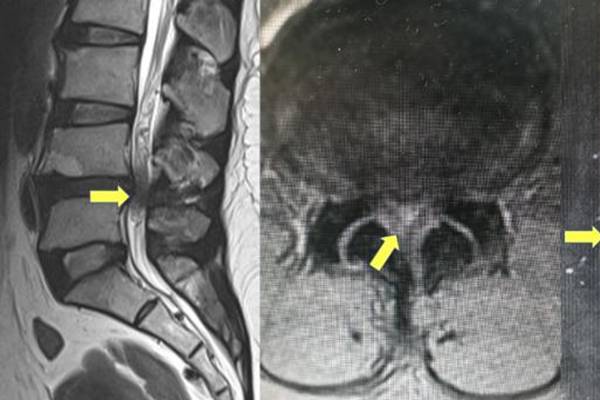
Image showing an MRI scan of a spinal stenosis case.
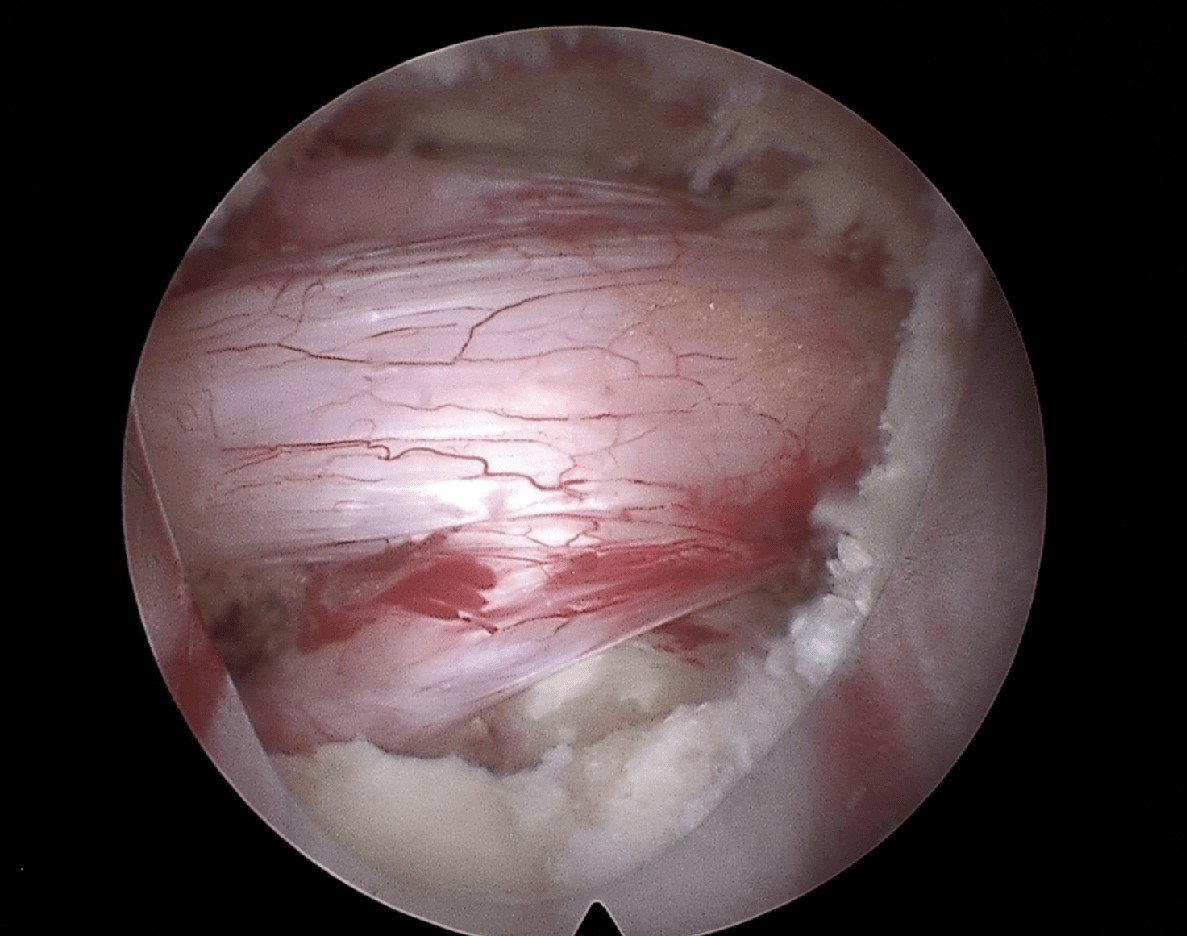
Image showing endoscopic surgery being used to treat spinal stenosis.
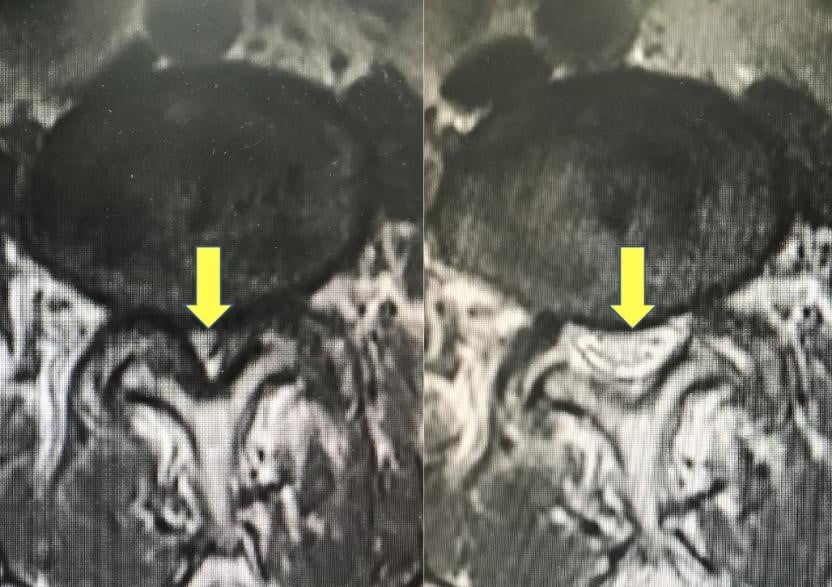
Image showing an MRI scan of a preoperative spinal stenosis case (left) and the postoperative MRI scan showing its improvement (right).
For more information please contact:
Last modify: May 09, 2025