The 2026 American Guidelines for ERCP Quality and Safety: What Patients Should Know Before Their Procedure
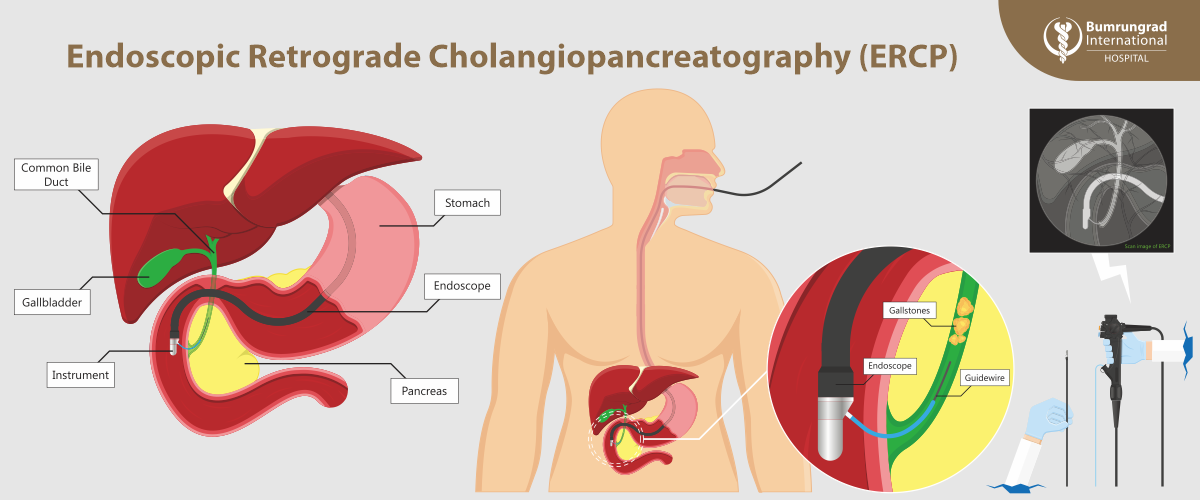
Endoscopic Retrograde Cholangiopancreatography (ERCP) is one of the most technically demanding procedures in gastroenterology. It combines endoscopy with real-time X-ray imaging to diagnose and treat diseases of the bile ducts and pancreas. Because ERCP carries higher risks than standard endoscopy, the
American College of Gastroenterology (ACG) and the
American Society for Gastrointestinal Endoscopy (ASGE) updated
2026 Quality and Safety Guidelines to define what constitutes
high-quality ERCP care.
If you or a loved one are scheduled for ERCP, this guide explains what patients should expect from a high-quality center in 2026.
Part 1: Ensuring ERCP Is Truly Necessary
ERCP is Primarily a Therapeutic Procedure, Not a Diagnostic Test
A key quality indicator is deciding
whether ERCP is needed at all. Modern guidelines emphasize that ERCP should be used
only to treat confirmed problems, not to “look around.”
Appropriate Indications for ERCP
High-quality centers perform ERCP for clear, evidence-based reasons, including:
- Obstructed bile ducts, such as bile duct stones (choledocholithiasis) or tumors requiring stent placement
- Bile leaks, commonly after gallbladder surgery
- Selected pancreatic conditions, including duct leaks or specific forms of chronic pancreatitis
Red flag: Recommending ERCP without prior imaging (ultrasound, CT, or MRI) does not meet current quality standards.
Part 2: Non-Invasive Testing Comes First
- Modern ERCP guidelines strongly recommend “non-invasive first” diagnostics: MRCP (Magnetic Resonance Cholangiopancreatography): A specialized MRI providing detailed 3D images of bile and pancreatic ducts without pancreatitis risk
- EUS (Endoscopic Ultrasound): Allows detection of very small stones or tumors missed by CT scans
This “non-invasive first” approach reduces unnecessary ERCP-related complications.
Part 3: Meaningful Informed Consent
High-quality care requires more than a signature —it requires
clear communication and patient understanding. Patients must understand the
five major ERCP risks:
- Pancreatitis (most common complication)
- Bleeding, especially after sphincterotomy
- Infection, including cholangitis
- Perforation of the digestive tract
- Sedation or anesthesia-related risks
Part 4: Preparation Before the Procedure
Medication Review
A quality team reviews medications at least one week in advance, including:
- Blood thinners, to reduce bleeding risk
- Diabetes medications, due to fasting requirements
- Weight-loss or metabolic drugs such as semaglutide or tirzepatide, which may delay gastric emptying and increase aspiration risk
Antibiotic Use Is Selective
Antibiotics are recommended only when:
- Complete bile drainage may not be possible
- The patient is immunocompromised or has specific heart valve conditions
- The patient has primary sclerosing cholangitis (PSC)
Part 5: Technical Quality During ERCP
Cannulation Success
- Quality benchmark: Successful duct access in over 90 percent of patients with normal anatomy
- Fewer attempts reduce the risk of pancreatitis
Stone Clearance
- Goal: Complete bile duct stone removal in over 90 percent of standard cases
- Advanced centers use techniques such as large balloon dilation and SpyGlass cholangioscopy with laser lithotripsy for complex stones
Radiation Safety
- ERCP uses fluoroscopy
- High-quality centers follow the ALARA principle (As Low As Reasonably Achievable) to minimize radiation exposure
Part 6: Preventing Post-ERCP Pancreatitis (PEP)
Rectal NSAIDs
Routine use of rectal indomethacin or diclofenac:
- Reduces severe pancreatitis risk by nearly 50 percent
- Should be used unless contraindicated
Temporary Pancreatic Stents
- Used when pancreatic irritation risk is high
- Help maintain pancreatic duct drainage and usually pass spontaneously or are removed later
Part 7: Recovery, Follow-Up, and Outcomes
Unplanned Hospital Visits
- Quality target: Less than 15% unplanned ER visits or admissions within 14 days
Thirty-Day Follow-Up
High-quality ERCP care includes:
- Tracking and reporting all complications
- Clear communication of biopsy and pathology results
Warning Signs After ERCP
Patients should seek immediate care for:
- Severe or worsening abdominal pain
- Fever or chills
- Black or tarry stools
- Chest pain or difficulty swallowing
Why Choosing the Right Center Matters
High-quality ERCP begins well before the procedure itself. Institutions that prioritize
non-invasive diagnostics, strict adherence to quality benchmarks, and proactive complication prevention consistently achieve better outcomes.
At
Bumrungrad International Hospital, ERCP is performed within an evidence-based clinical pathway aligned with the 2026 ACG and ASGE quality indicators. Procedures are led by U.S.-trained advanced endoscopists educated under guideline authors and supported by a fully integrated multidisciplinary team, advanced technologies such as SpyGlass cholangioscopy, and comprehensive post-procedure monitoring.
In complex biliary and pancreatic disease, optimal outcomes arise when
clinical judgment, technical expertise, and institutional standards are aligned with a single global definition of excellence.
Frequently Asked Questions (FAQ)
1. What is ERCP used for?
ERCP is used to treat bile duct and pancreatic duct conditions, such as stones, strictures, leaks, and certain tumors. It is not recommended for diagnostic purposes alone.
2. Is ERCP considered high risk?
ERCP has higher risks than standard endoscopy, particularly pancreatitis. Following 2026 quality guidelines significantly reduces complications.
3. How can patients reduce ERCP risks?
Choosing a high-quality center, ensuring non-invasive imaging is done first, using rectal NSAIDs, and following post-procedure instructions all lower risk.
4. How long is recovery after ERCP?
Most patients recover within a few days, but some complications can occur up to 2 weeks. Monitoring symptoms and follow-up are essential.
By Tossapol Kerdsirichairat, MD, FACG, FASGE
Clinical Associate Professor of Medicine
Advanced/Bariatric Endoscopy, Digestive Disease Center
Bumrungrad International Hospital
For more information please contact:
Last modify: February 06, 2026