Glaucoma: The Silent Thief of Sight
Imagine losing your vision without warning, no pain, no obvious symptoms, just a gradual narrowing of what you see until the world around you begins to fade. This is the reality of
glaucoma, often called the
“silent thief of sight.”
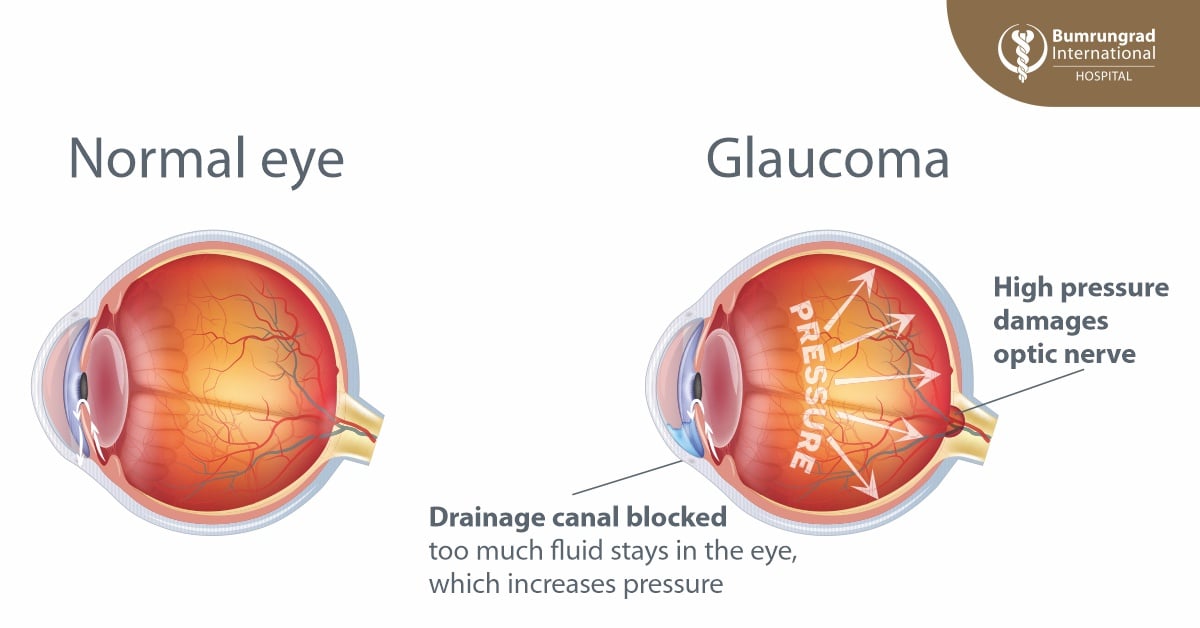
Glaucoma is not a single disease but a group of conditions that slowly damage the optic nerve, the pathway that carries images from the eye to the brain. This usually happens when the natural fluid in the eye doesn’t drain properly, causing pressure to build up. Over time, this pressure damages the delicate nerve fibers, leading to vision loss.
Why glaucoma matters globally
Glaucoma is not just an eye condition, it is a growing worldwide health challenge. Today, more than
80 million people over the age of 40, or about
3.5% of the global adult population, are living with the disease. And the numbers are climbing. By
2030, nearly
95 million people are expected to be affected.
The consequences are serious. Glaucoma has become the
second-leading cause of blindness globally, leaving around
8 million people bilaterally blind. Because vision loss from glaucoma is permanent, these figures highlight a critical truth: only
early awareness and timely detection can help preserve sight and prevent blindness on a global scale.
The main types of glaucoma
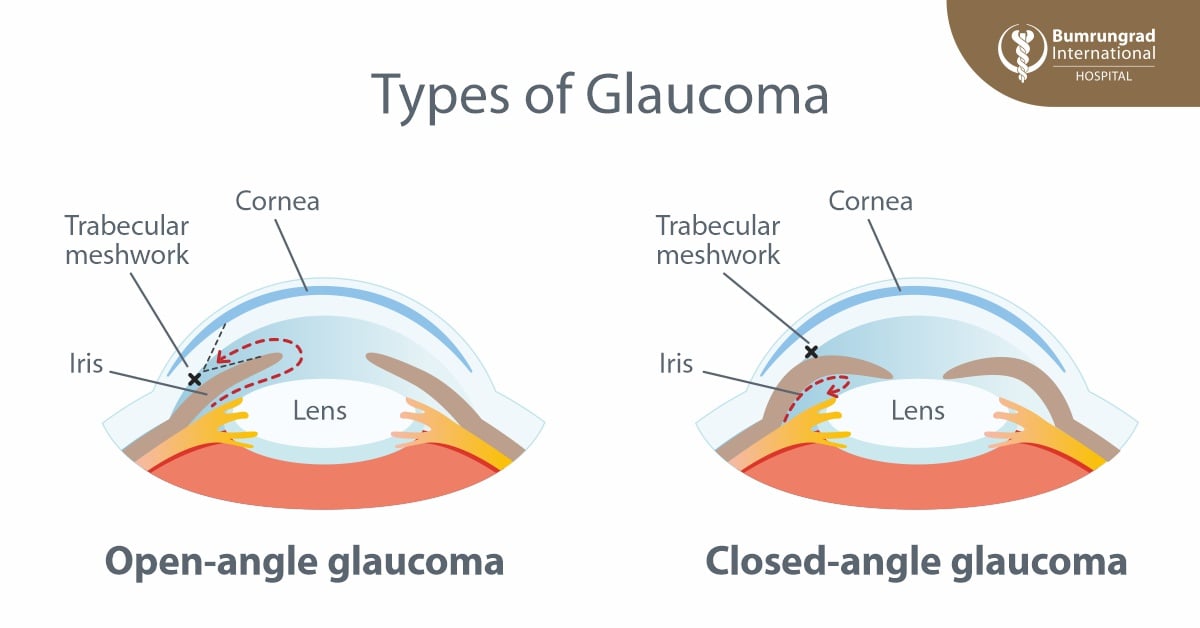
- Primary Open-Angle Glaucoma (POAG):
The most common type worldwide. The eye’s drainage canals gradually become less efficient, leading to a slow increase in eye pressure. Vision loss develops gradually and is often unnoticed until significant damage has occurred.
- Primary Angle-Closure Glaucoma (PACG):
More common in Asia. The drainage angle narrows or closes suddenly, causing a sharp rise in eye pressure. This form can lead to rapid and severe vision loss if not treated promptly.
Glaucoma symptoms: Early warning signs and emergencies
One of the most dangerous things about glaucoma is that it often develops
without any symptoms in its early stages. In fact, studies show that
up to half of people with glaucoma may not even know they have it. Symptoms usually appear only after the disease has already caused
irreversible optic nerve damage.
Common glaucoma symptoms
As glaucoma progresses, some people may notice:
- Eye pain or pressure
- Headaches
- Red or bloodshot eyes
- Blurred or double vision
- Gradual loss of peripheral vision (tunnel vision)
- Gradually developing blind spots (scotomas)
- Overall reduced or low vision
Emergency symptoms of angle-closure glaucoma
Certain types of glaucoma, particularly
acute angle-closure glaucoma, can cause sudden and severe symptoms that require
immediate medical attention to prevent permanent vision loss. These include:
- Severe eye pain with nausea or vomiting
- Rainbow-colored halos around lights
- Sudden loss of vision or flashing lights (photopsias)
- Rapid increase in floaters in your vision
- Blood pooling in front of the iris (hyphema)
- Bulging or enlarged eyeballs (buphthalmos)
If you experience any of these sudden glaucoma symptoms, seek emergency eye care right away. Prompt treatment can mean the difference between saving and losing your vision.
Glaucoma screening: Who is at risk and when to get tested
Because glaucoma usually develops without symptoms,
screening is the only way to catch it early. Specialists recommend:
- From age 40: Routine eye exams every 1–2 years.
- High-risk individuals: Annual exams are essential for people with
- a family history of glaucoma
- high eye pressure
- diabetes, hypertension
- severe near-sightedness
- thin corneas
- of Asian or African descent
- After age 60: Even without risk factors, yearly screening is strongly advised, as the risk increases significantly with age.
- Children and young adults: While rare, congenital or juvenile glaucoma can occur, and those at risk should be evaluated by an eye specialist.
- Individuals taking medications that increase eye pressure, such as steroids
- Individuals with a history of eye injury or eye surgery
How glaucoma is detected
Modern ophthalmology offers several advanced tools to detect glaucoma early:
- Slit Lamp Examination:
A central tool in glaucoma diagnosis. The doctor uses a special microscope with a bright light to look closely at the inside of your eye. With this test, they can see the optic nerve and the drainage angle—two areas often affected by glaucoma. Sometimes, your pupils may be dilated for a better view, and in certain cases, another test called gonioscopy is done to examine the drainage angle in even greater detail.
- 24-2 Visual Field Testing:
A standard test measuring the central 24 degrees of vision using 54 light points to reveal early blind spots.
- Optical Coherence Tomography (OCT):
A painless, high-resolution imaging scan that shows microscopic changes in the retina and optic nerve before symptoms appear.
- Fundus Photography:
A detailed photograph of the back of the eye, including the retina, optic nerve, and blood vessels. This test provides a visual record that helps doctors monitor changes in the optic nerve over time and detect signs of glaucoma progression.
Treatment and management
Glaucoma cannot be cured, but its progression can often be slowed or stopped with the right treatment. Options include:
- Prescription eye drops to lower intraocular pressure.
- Laser therapy to improve drainage.
- Minimally invasive or traditional surgery for advanced cases.
With early diagnosis and proper care, many people with glaucoma can maintain useful vision throughout their lives.
Learn more about glaucoma screening at Bumrungrad
Early detection is the best defense against glaucoma.
Bumrungrad International Hospital’s Eye Excellence Center offers a comprehensive screening, which includes advanced tests such as:
- Visual acuity and auto refraction tests to measure how clearly you see and detect any refractive errors.
- Tonometry to check eye pressure, one of the most important risk factors for glaucoma.
- Central corneal thickness (CCT) measurement, since thinner corneas can mask dangerously high eye pressure.
- Slit lamp biomicroscopy, allowing the doctor to closely examine the front of the eye and drainage angle.
- Computerized visual field testing to detect early blind spots that may not yet affect daily vision.
- Fundus photography with an ultra-widefield digital retinal camera (CLARUS), providing detailed images of the retina and optic nerve for long-term monitoring.
- Optical Coherence Tomography (OCT) of the optic nerve head and macula, a high-resolution scan that detects microscopic changes before symptoms appear.
These state-of-the-art tools allow our specialists to detect glaucoma at its earliest stages, before symptoms appear, and create a personalized care plan for each patient.
FAQs about glaucoma
What is glaucoma?
Glaucoma is a group of eye diseases that damage the optic nerve, usually due to increased eye pressure. It develops silently without symptoms in early stages, earning the name
“silent thief of sight.” If untreated, it can lead to permanent and irreversible vision loss.
Who is most at risk for glaucoma?
People over 40, those with a family history of glaucoma, individuals with diabetes or high blood pressure, and people of Asian or African descent are at higher risk. Severe near-sightedness and thin corneas also increase risk. Regular eye screenings are essential for these groups.
What are the symptoms of glaucoma?
In its early stages, glaucoma usually causes no symptoms—that’s why many people don’t know they have it. As the disease progresses, signs may include eye pain or pressure, blurred or double vision, headaches, red eyes, tunnel vision, or blind spots.
What are emergency symptoms of glaucoma?
Some types, especially acute angle-closure glaucoma, can cause sudden symptoms that require urgent treatment. Warning signs include severe eye pain with nausea or vomiting, rainbow-colored halos around lights, sudden vision loss, flashing lights, or blood pooling in front of the iris. Immediate medical attention is critical to prevent permanent blindness.
Can glaucoma cause blindness?
Yes. Glaucoma is the
second-leading cause of blindness worldwide, responsible for around 8 million cases of complete bilateral blindness. Because vision loss is irreversible, early detection and treatment are critical to prevent blindness and preserve eyesight.
How is glaucoma detected?
Glaucoma is detected with specialized eye exams such as
slit lamp examination,
visual field testing,
Optical Coherence Tomography (OCT), and
fundus photography. These tests allow doctors to spot early damage to the optic nerve and retina—often before vision is affected.
How often should I be screened for glaucoma?
Adults should start glaucoma screenings at age 40, every 1–2 years. After age 60—or if you have risk factors like family history, diabetes, or high blood pressure, annual exams are strongly recommended. Early screening is the only way to protect vision from silent damage.
Can vision lost from glaucoma be restored?
No. Once glaucoma damages the optic nerve, vision loss is permanent and cannot be reversed. However, treatments such as eye drops, laser therapy, and surgery can slow or stop disease progression, helping patients preserve their remaining vision.
For more information please contact:
Last modify: December 22, 2025